The How and Why of Plagiocephaly and Other Forms of Acquired Head Flattening
Posted on by Gary F. Rogers, M.D., J.D., LL.M., M.B.A., M.P.H.
 A common question I am asked by parents is how head flattening occurs and why it only occurs in some infants (25-35% by most estimates). First, let’s address why it only affects some infants.
A common question I am asked by parents is how head flattening occurs and why it only occurs in some infants (25-35% by most estimates). First, let’s address why it only affects some infants.
Risk Factors for Head Flattening in Babies
The risk factors for head flattening can be placed into three major categories- torticollis, prematurity, and developmental delay- each of which affects the infant’s ability to “self-reposition” the back of their head. The most important is torticollis, a cervical muscle imbalance that restricts independent head mobility early in life. This condition is classically described as a head tilt to one side and chin rotation to the other with or without a palpable mass in the sternocleidomastoid muscle, but the presentation can be far more subtle. Early in life, the most common presentation is a strong head rotation preference, which should be assumed to be torticollis until proven otherwise. This finding should prompt a referral to a physical therapist for a formal evaluation.
Causes of Flat Head in Babies
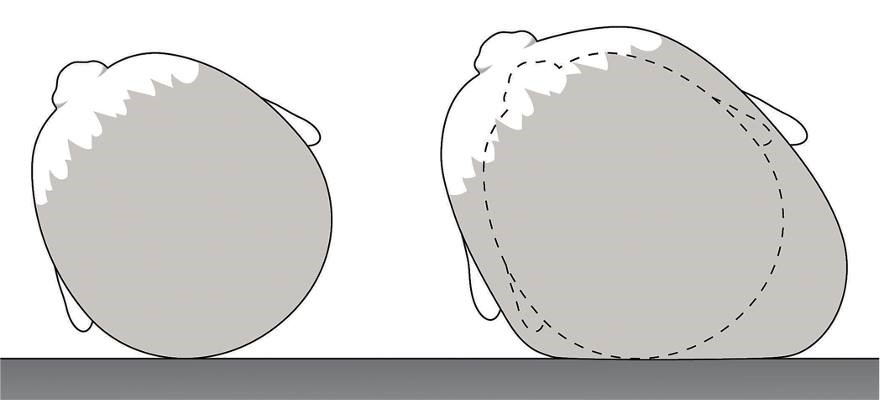
Now let’s consider how head flattening occurs. For infants that have a risk factor like torticollis, they will tend to keep the head in one position and as it grows against the typically flat resting surface, it gradually grows flatter. The process has nothing to do with a "soft" head or that the bones are malleable. It is exclusively a result of growth displacement around a point of contact. Newton's Law (equal and opposite forces) predicts that the force (weight x gravity) applied by the infant's head to the bed is met with an equal upward force from the bed to the head. This pressure restricts growth in the area of contact and growth is displaced to any area where there is no contact. As the head grows and increases in weight, this process accelerates. This is why head flattening becomes very apparent between 6-8 weeks in prone kids. As long as the head contacts the bed in the same spot, this process will continue. This is effectively a race between resolution of torticollis and progression of head flattening.
If the torticollis is mild, and motor development is normal, the progression of head flattening may stop quickly as the child begins to move the head more freely and redistributes the point of contact to other areas of the posterior cranium. Redistributing contact pressure to multiple areas, and not just one, is the whole objective of reposition efforts, physical therapy, and tummy time (attempts to accelerate the development of motor control). For kids with more severe torticollis, or with developmental delays, these modalities can take much longer to work and flattening can become quite severe. Infants with significant torticollis often resist repositioning and tummy time, unfortunately, and it is very hard to predict up front how these efforts will affect head shape. The wide variation in risk factor severity and type means that what works for some families (repositioning, TT, PT) may not work for others. Most parents who ultimately seek out treatment for their infant’s head flattening have tried all of these modalities only to find that their child's head continued to worsen. It cannot be assumed that they did it wrong or did not follow instructions. Instead, they are fighting a very different set of circumstances.
How to Treat Head Flattening
I have 4 children and never did anything to reposition or try to prevent head flattening, yet my kids maintained a wonderful head shape. Why? Simple- none of them had torticollis and all were developmentally appropriate for their age. My two brothers each had children who became flat in infancy. The difference? They had torticollis and I could see that from day one. Neither of my brothers listened to my concerns and after 3 months, both of their kids had varying degrees of head flattening. The key to identifying which kids will develop head flattening is to identify and manage the risk factors (e.g., a strong head rotation preference) early and intervene before the flattening progresses.
There are some options available if you are interested in treating patients with head flattening. Depending on the severity and the age of the patient, there is the Perfect Noggin, an ergonomic and clinically effective sleep surface available to maintain a natural head shape in infants. For older infants the Boston Band, a cranial remolding orthosis manufactured by Boston Orthotics & Prosthetics works well.
Learn more about the Perfect Noggin Learn more about the Boston Band
Gary F. Rogers, M.D., J.D., LL.M., M.B.A., M.P.H., is an academic pediatric plastic surgeon who specializes in various craniofacial anomalies, including plagiocephaly. He is a Professor of Pediatrics and Surgery at the George Washington School of Medicine, and holds the Johnston Family Endowed Chair in Pediatric Plastic Surgery. Dr. Rogers is Chief of the Department of Pediatric Plastic Surgery at Children's National Health System.
Sign up for more articles like this

